By Katie Hendry, Dr Lucyna Gozdzielewska and Prof Lesley Price
Effective hand hygiene among healthcare staff is one of the most important infection prevention strategies available worldwide. Hand hygiene also helps individuals to effectively reduce bacteria on their hands in their daily lives. However, uncertainty remains concerning a range of issues related to hand hygiene, including the most effective hand hygiene technique, the most optimal volume of the hand hygiene product that should be used, or the duration of hand hygiene.
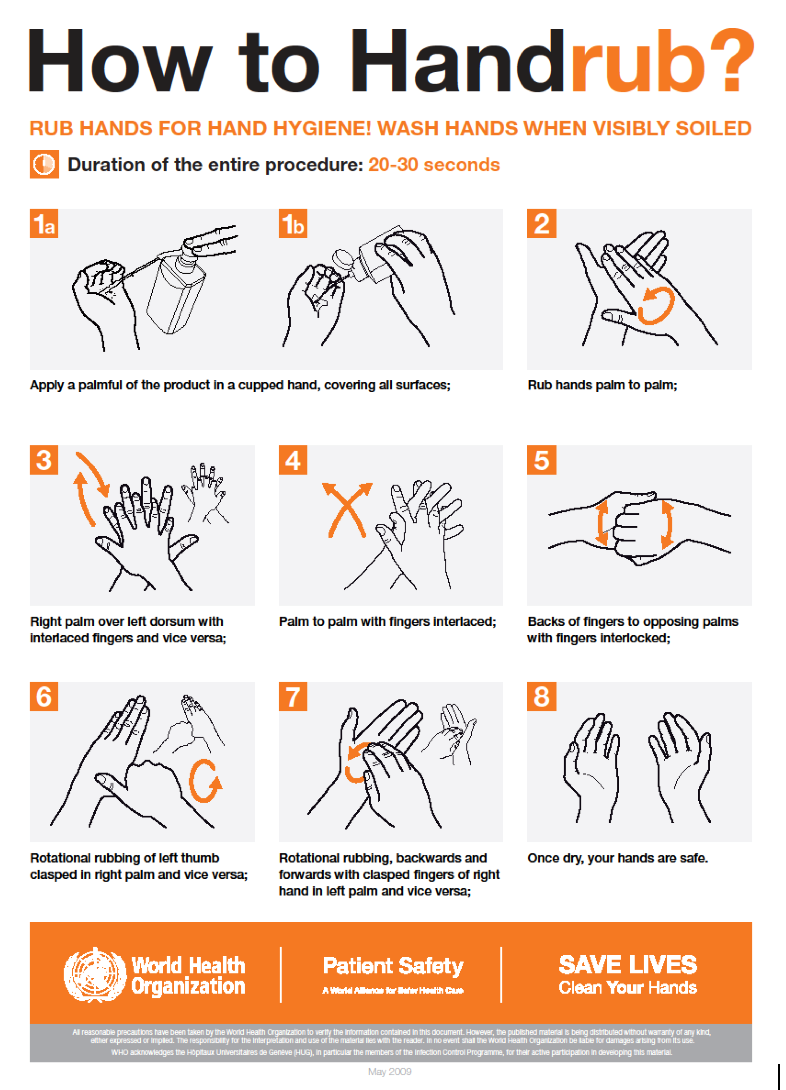
The World Health Organisation (WHO) recommends a specific hand hygiene technique, called the 6-step technique, using six defined steps to cover all hand surfaces when performing hand hygiene, either by handwashing with soap and water or by the application of alcohol-based hand rub (ABHR). However alternative techniques have been investigated.
For the application of ABHR, the WHO recommends a 20-30 second application time using a “palmful of the product, sufficient to cover all hand surfaces, while the Centers for Disease Control and Prevention indicates that the hands should be rubbed until dry for around 20 seconds, using the manufacturer-recommended volume of ABHR.
To address these uncertainties, we were funded by the WHO to update two systematic reviews. One of these reviews, examined the effectiveness of the WHO 6-step hand hygiene technique in reducing microbial load on hands and covering hand surfaces, and compared its effectiveness to other techniques, whereas the second updated review examined factors influencing the effectiveness of ABHR in healthcare, that is ABHR volume, application time or rubbing friction.
Our findings show that while the WHO 6-step technique does reduce the bacterial load on hands, the evidence was insufficient to identify the most effective hand hygiene technique. For example, one study found the 6-step technique was more effective than a simpler technique, involving the application of a product on hands and rubbing hands together until dry while covering all hand surfaces, whereas another study showed no difference between these two techniques. Other evidence showed that a simplified, 3-step technique, consisting of covering all surfaces of the hands followed by rubbing the fingertips against the opposite palm and rubbing both thumbs, was more effective than the 6-step technique in a laboratory setting, but not in a clinical setting. Yet another study found that an adapted version of the 6-step technique in which the sequence order of the steps was changed, was more effective than the original WHO 6-step technique.
With regards to the factors influencing the effectiveness of hand rubbing with ABHR, our findings showed that the larger ABHR volume was used, the longer it took to dry on hands and the greater reduction in bacterial load was observed but it was not possible to identify the most optimal ABHR volume that should be used or duration of hand rubbing. Only one study investigated rubbing friction. It showed that the application of sprayed ABHR without rubbing hands together was less effective in reducing bacteria on hands than poured or sprayed ABHR with hand rubbing performed, suggesting the importance of the rubbing friction.
Our reviews also showed that studies differed in many aspects in that they tested different ABHR volumes, application times, used different formulations of ABHR, and different techniques for their application. Furthermore, to measure the bacterial load on hands studies also differed in the methods used to collect microbiological samples from study participants’ hands, highlighting a need for standardization of research methods in future hand hygiene studies.
The findings from our updated reviews show that the evidence is insufficient to suggest changes to WHO current guidelines. Thus, until more evidence is available, healthcare workers should continue following the current WHO recommendations by using the 6-step hand hygiene technique, and when applying ABHR, doing so for 20-30 seconds using a “palmful of the product, sufficient to cover all hand surfaces”. Our findings also highlighted the need to standardise the protocols for conducting and reporting hand hygiene studies.
Our updated systematic review paper on the effectiveness of hand hygiene techniques was published in the American Journal of Infection Control and is available in full text to all: https://www.sciencedirect.com/science/article/pii/S0196655322000670, while the systematic review on factors influencing the effectiveness of alcohol‑based hand rubbing in healthcare was published in the Antimicrobial Resistance & Infection Control can be accessed by all using this link: https://aricjournal.biomedcentral.com/articles/10.1186/s13756-021-01049-9
To find out more about the SHIP team, head on to the GCU website, read the rest of our blogs and follow us on Twitter @SHIPGCU